All Things Hand & Upper Limb
Cubital Tunnel Syndrome & The Ulnar Nerve
Cubital Tunnel Syndrome & The Ulnar Nerve
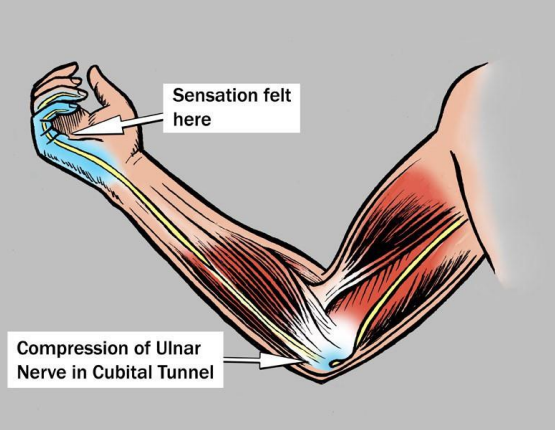
Do you find that the inside of your elbow hurts? Do you find that you ring and little finger experiences pins and needles? Does your pain wake you up at night? Or does it feel like you have hit your funny bone? If that’s the case you might have an ulnar nerve compression otherwise known as cubital tunnel syndrome. Cubital tunnel syndrome is the second most common compression neuropathy in the upper limb after carpal tunnel syndrome (DeGeorge & Kakar, 2019). If left untreated it can result in long term deficits and a reduction in function of your arm and hand. The most common presentations of cubital tunnel syndrome include sensory and motor deficits with or without muscle atrophy (wastage) of the arm and hand.
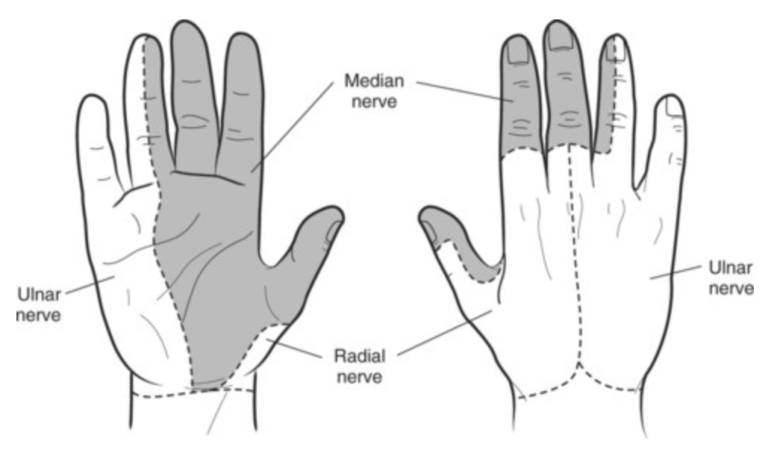
To better appreciate cubital tunnel syndrome, we need to understand the anatomy and nerves of the upper limb and how they function within the body. The brachial plexus, is a network of nerves in the shoulder that carries movement and sensory signals from the spinal cord to the arms and hands. Within that network is the ulnar nerve. The ulnar nerve is a single nerve that runs on the inside of the arm that travels behind the medial (inside) epicondyle all the way down to the hand, supplying sensation to the muscles of the forearm and hand along the way (Gilcrease-Garcia, Deshmukh & Parsons, 2020)
Assessment
To ensure that the correct condition is being treated a thorough assessment needs to be completed to confirm your diagnosis. There are a number of ways this can be completed (Daniels, Mintz, Endo, Dines & Sneag, 2019).
- Assessment from your Hand therapist
- Radiologically from scans such as
- A nerve conduction study – measures how fast an electrical impulse moves through your nerve and whether there is a latency or not.
- Ultrasound – to assess for any swelling or tenosynovitis of the surrounding soft tissues
Treatment
When the nerve is compressed rehabilitation and interventions can assist in alleviating symptoms. This can be done in either a conversative manner with your Hand therapist or surgically if required.
Conservative management
- Treatment of ulnar nerve begins with a thorough assessment of the upper limb to determine where the nerve may be affected, what symptoms you present with and how they are affecting your daily living.
- Following assessment your Hand therapist may recommend custom bracing to offload the ulnar nerve during the day and/or overnight. This allows the irritated nerve to rest and become less irritable.
- Once appropriate and irritability has decreased your hand therapist will prescribe you an individualised home exercise program that focuses on de-sensitisation, nerve gliding, pain management and graded strengthening to assist you on your road to recovery.
Non-conservative:
- When non-conservative treatment fails to cure your symptoms referral to a surgeon can be facilitated, the most common surgery that is completed is an ulnar nerve transposition
- During surgery, a small incision is made around the medial epicondyle and the surgeon will locate the ulnar nerve. The nerve is then moved out of its location under the medial epicondyle and placed in a more superficial area on the front the medial epicondyle. This new position may be directly under the skin or may be within a muscle. This process of moving the ulnar nerve out of the groove enables the nerve to move freely and help to restore upper limb functioning (Said, Van Nest, Foltz & Ilyas, 2019).
- Following surgery, Hand therapy is indicated to assist with wound care, scar management and rehabilitation involving range of motion, nerve gliding exercises and safe graded strengthening.
Evidence has shown that the sooner the treatment and management is sought out the better the long-term prognosis for any individual. If you feel that you are experiencing any of the above symptoms you should seek out assistance from your Hand therapist.
References
http://www.brainspinecentre.com.au/ulnar-nerve-decompression-at-elbow.html
Daniels, S. P., Mintz, D. N., Endo, Y., Dines, J. S., & Sneag, D. B. (2019). Imaging of the post-operative medial elbow in the overhead thrower: common and abnormal findings after ulnar collateral ligament reconstruction and ulnar nerve transposition. Skeletal Radiology, 48(12), 1843-1860.
DeGeorge Jr, B. R., & Kakar, S. (2019). Decision-making factors for ulnar nerve transposition in cubital tunnel surgery. Journal of wrist surgery, 8(02), 168-174.
Ulnar Nerve Entrapment at the Elbow
Gilcrease-Garcia, B. M., Deshmukh, S. D., & Parsons, M. S. (2020). Anatomy, imaging, and pathologic conditions of the brachial plexus. Radiographics, 40(6), 1686-1714.
Said, J., Van Nest, D., Foltz, C., & Ilyas, A. M. (2019). Ulnar nerve in situ decompression versus transposition for idiopathic cubital tunnel syndrome: an updated meta-analysis. Journal of Hand and Microsurgery, 11(01), 018-027.